Uveitis Case #3
Authors: Carolin Aizouki (1), Dr. Alexander Kaplan (2)
Affiliations: (1) University of Alberta (2) University of Toronto
ID: 42M, painless, progressive vision loss OD for 6 weeks.
Past Ocular History: None
Ocular gtts: None
Relevant Medical History: None, non-smoker. No recent travel, no childhood exposure to TB, no cough or SOB.
-
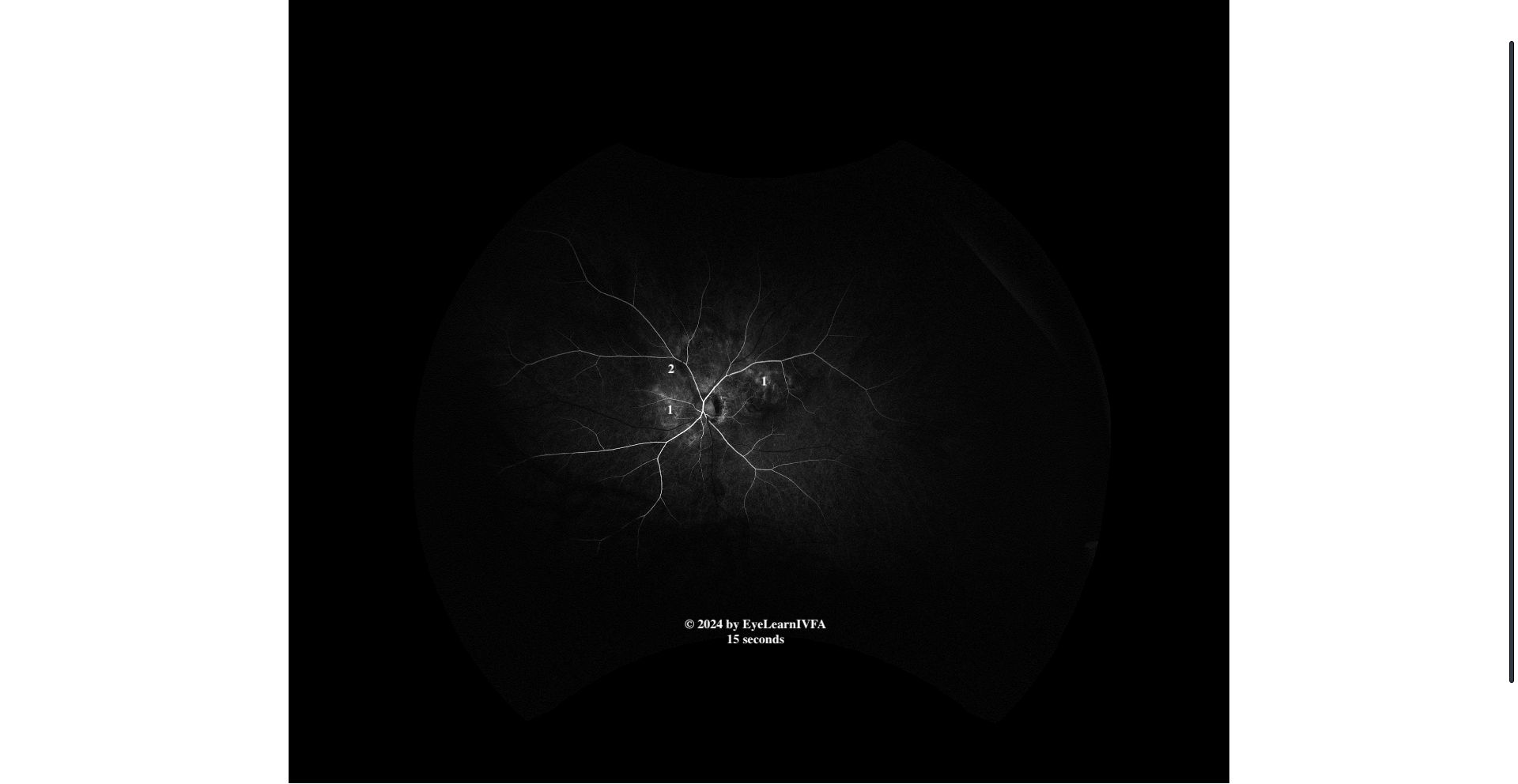
IVFA OS at 15 seconds
Arterial phase
Key features include:
Irregular, ill-defined patchy areas of hyper-fluorescence (1) and hypofluorescence (2) in a peripapillary disruption.
-
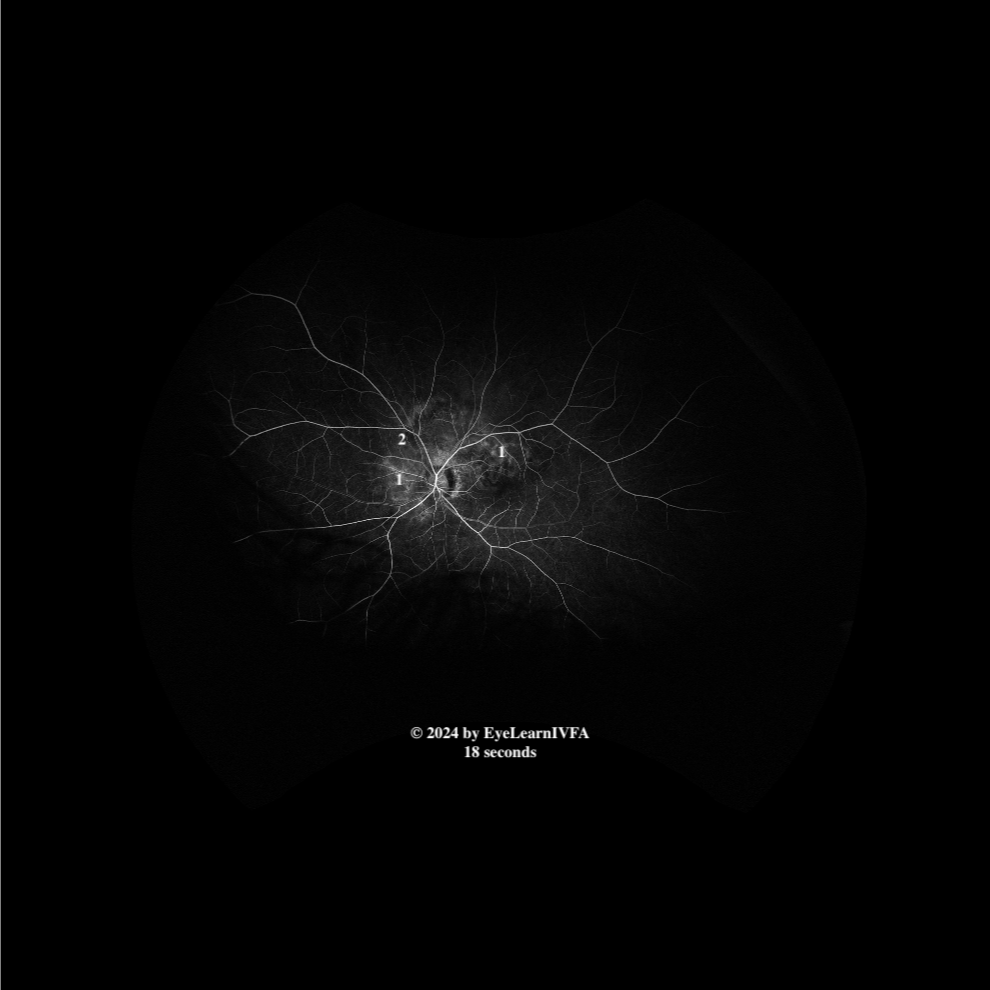
IVFA OS at 18 seconds
Early to mid arteriovenous phase.
Key features include:
Subtle areas of hypofluorescence (2), with increasing surrounding marginal fluorescence, again respecting a peripapillary disruption (1).
No obvious retinal vessel staining to indicate vasculitis.
-
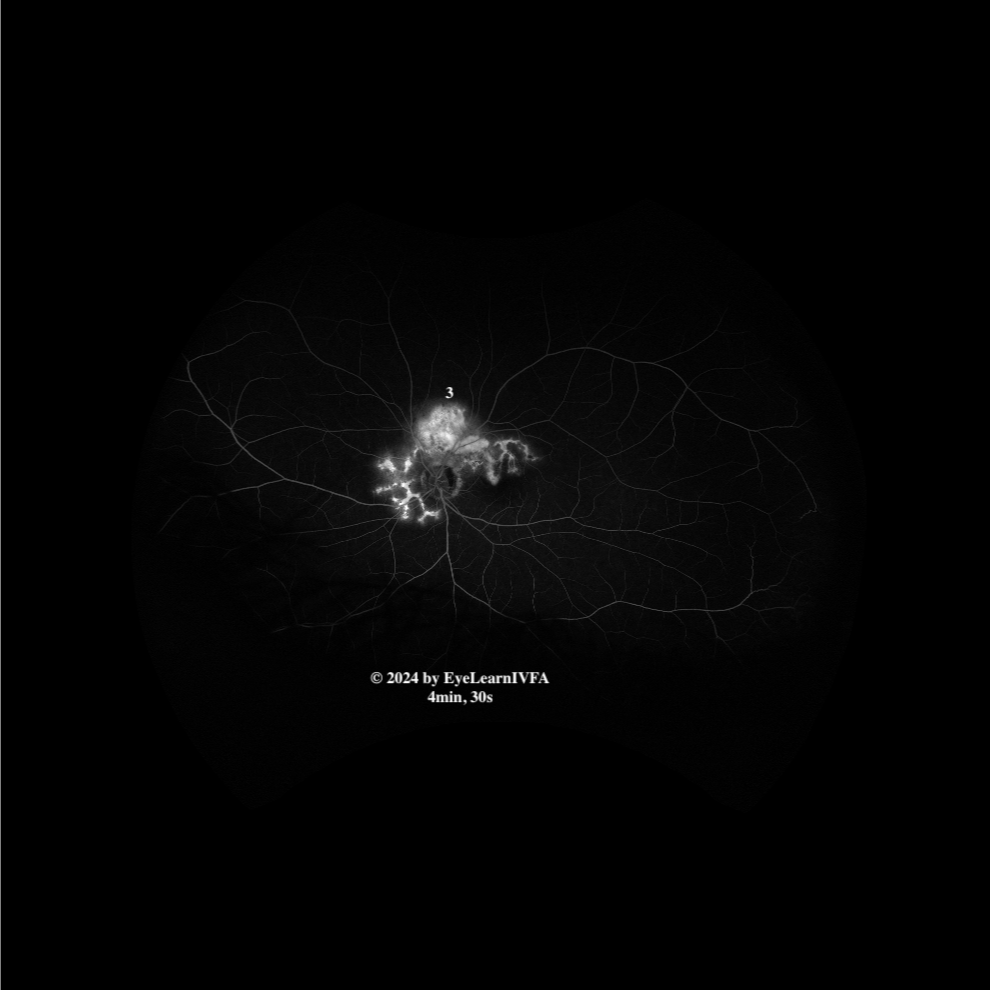
IVFA at 4 minutes 30 seconds
Late Phase
Key features include:
Evident serpentine shape.
Increased intensity and more uniform hyperfluorescence (1) due a mix of leakage and staining over the scar.
Evidence of late leakage superior to the disc, retinal hemorrhages on fundus photos, and subretinal fluid on OCT points to CNVM in that location (3).
-
Serpiginous choroiditis. Late hyperfluorescence from staining, in the peripapillary distribution is characteristic of classic serpiginous choroiditis. The presence of subretinal fluid on OCT along with retinal hemorrhages on fundus photos, and late leakage superior to the disc on IVFA indicates CNVM in that location. This suggests the case involves a fibrovascular scar that is active a secondary CNVM.
-
Serpiginous-like choroiditis from Tuberculosis
AMPPEE
Ampiginous choroiditis/ Relentless Placoid Choroiditis
Multifocal choroiditis
Toxoplasmosis
Syphilitic chorioretinitis
-
IVFA is a valuable tool in serpiginous choroiditis, despite the choroid often being better characterized on ICGA. The Optos fundus photo demonstrates geographic areas of chorioretinal atrophy extending in a serpiginous pattern from the optic disc. Corresponding OCT shows subretinal fluid with an irregular, ragged inner surface. Further elucidation of these findings with IVFA was pursued. IVFA in serpiginous choroiditis usually has early hypofluorescence, with progressive marginal fluorescence and then late hyperfluorescence. It can help to characterize the lesion's extent and pattern confirming a serpentine or geographic lesion that implicates the peripapillary and macular regions. It can delineate active versus more atrophic/intactive lesions based on the amount of observed staining and leakage. Classic patterns of IVFA help to differentiate it from other infectious and non-infectious causes on the differential. As well, IVFA can identify choroidal neovascular membranes, a potential complication of serpiginous choroiditis.
-
Nazari Khanamiri H, Rao NA. Serpiginous Choroiditis and Infectious Multifocal Serpiginoid Choroiditis. Survey of Ophthalmology. 2013 May;58(3):203–32.
Ahmed AH, Kubaisi B, Foster CS. Serpiginous Choroiditis. JAMA Ophthalmology. 2017 Apr 13;135(4):e165495.