Uveitis Case #1
Authors: Kevin Ly (1), Dr. Alex Kaplan (2)
Affiliations: (1) University of Alberta (2) University of Toronto
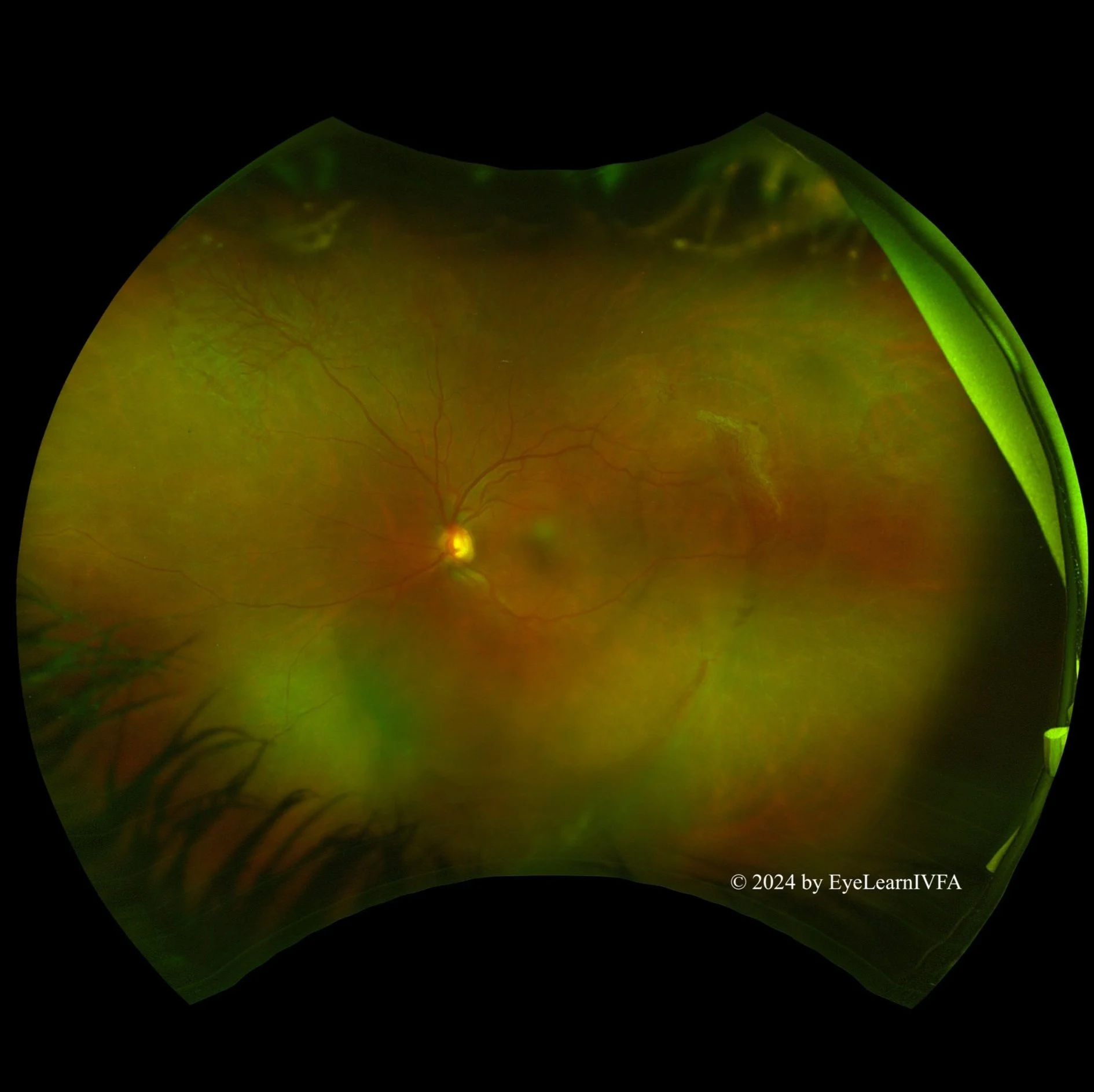
ID: 37F, blurred vision and floaters x 2 months.
Past Ocular History:
Granulomatous Acute Anterior Uveitis (Treated 2 years ago)
No ocular surgery, no ocular trauma.
Ocular gtts: Prednisolone Acetate QID x4 weeks
Relevant Medical History: immunocompetent - investigations for infectious, inflammatory, and neoplastic causes of uveitis returned negative.
-
IVFA at 19 seconds
Early Arteriovenous Phase (early laminar flow).
Key features include:
Capillary drop-out/non-perfusion (1).
At the edges of the remaining perfused retina, neovascular bundles temporally and superonasally (2).
Vascular architecture and perfusion of macula remains intact.
-
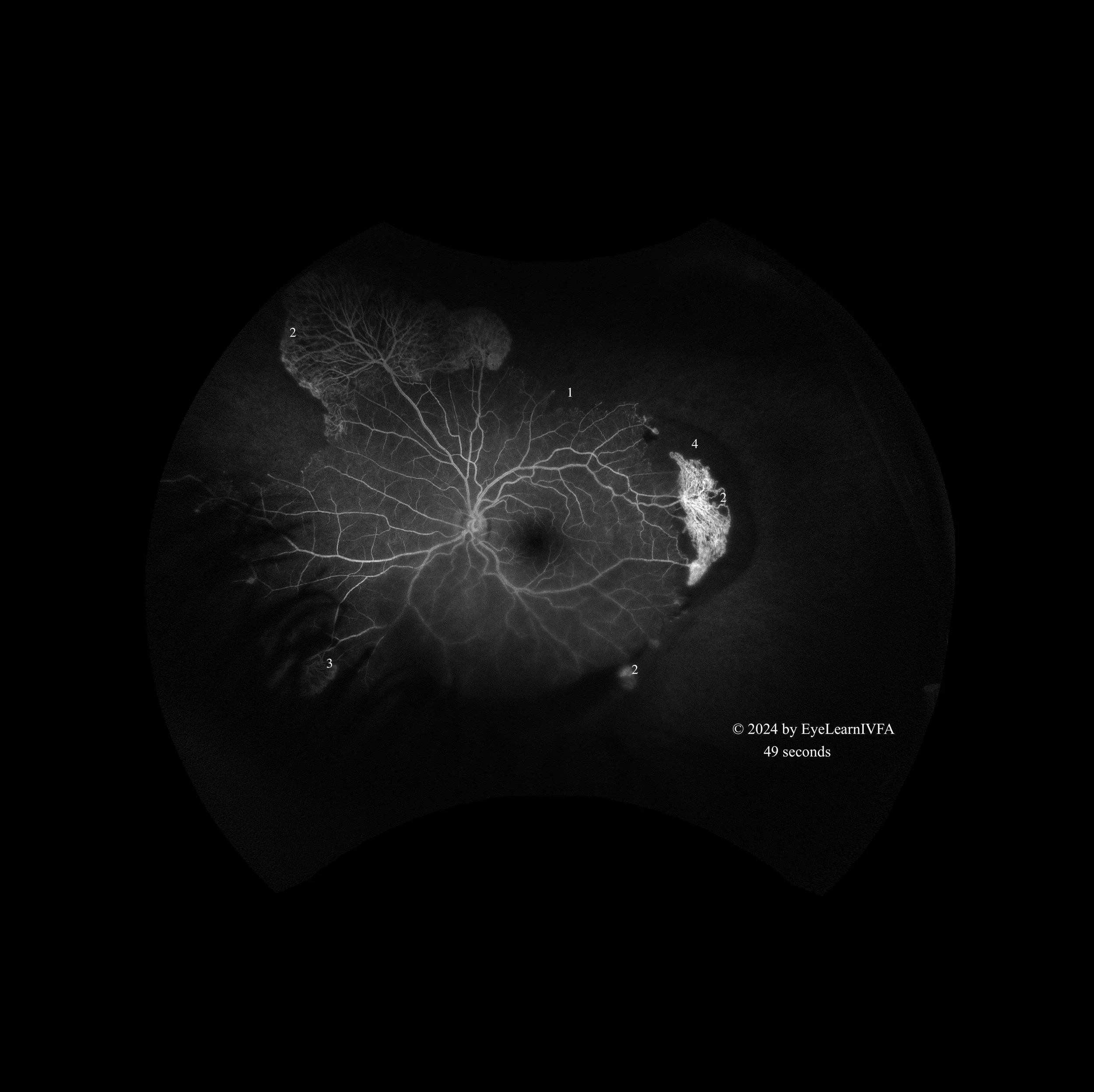
IVFA at 49 seconds
Mid-Late Arteriovenous Phase
Key features include:
More apparent peripheral retinal capillary drop-out/non-perfusion nearly 360 degrees (1).
Increased intensity of hyperfluoresence of superonasal sea-fan like neovascularization, temporal retinal neovascularization and smaller neovascular bulbs (2).
Inferonasal sea-fan like neovascularization underneath the lashes (3).
Hypofluoresence from sub-retinal fluid blocking underlying choroidal fluorescence (4).
-
IVFA a 3 minutes 42 seconds
Late Phase
Key features include:
Increasing hyperfluorescence (intensity and size) of previously mentioned areas of neovascularization, secondary to leakage (1).
Hyperfluorescent optic nerve (2).
Maintained areas of capillary drop-out and non-perfusion throughout the angiogram secondary to occlusive disease (3).
-
The constellation of reduced vision, intra-ocular inflammation, areas of non-perfusion with secondary neovascularization on IVFA supports the diagnosis of occlusive retinal vasculitis.
-
Systemic inflammatory disease (e.g. SLE, Behçet’s, sarcoidosis)
Infectious retinitis
CMV, HSV, VZV
Tuberculosis
Toxoplasmosis
Syphilis
Retinal vein occlusion
Retinal artery occlusion
Diabetic retinopathy
Ocular ischemic syndrome
Susac’s syndrome
Idiopathic retinal vasculitis, aneurysms, and neuroretinitis (IRVAN)
-
The IVFA characterizes the extent of the occlusive vasulitis. It confirms peripheral non-perfusion, demonstrates areas of secondary neovascularization that are often challenging to see on fundus exam. It also shows involvement of the optic nerve which is not obvious by fundus examination (1-4).
-
Rosenbaum JT, Sibley CH, Lin P. Retinal vasculitis. Curr Opin Rheumatol. 2016 May;28(3):228–35. doi:10.1097/BOR.0000000000000271.
Agarwal A, Rübsam A, zur Bonsen L, Pichi F, Neri P, Pleyer U. A Comprehensive Update on Retinal Vasculitis: Etiologies, Manifestations and Treatments. Journal of Clinical Medicine. 2022 Apr 30;11(9):2525. doi:10.3390/jcm11092525.
1.Arora A, Agarwal M, Chieh Loh N, Amin H, Menia NK, Agrawal R, et al. Diagnostic Workup of Retinal Vasculitis: An Algorithmic Approach. Ophthalmologica. 2024 Sep 5;247(5-6):280–92. doi:10.1159/000541149.
Abu AM, Herbort CP, Tabbara KF. A clinical approach to the diagnosis of retinal vasculitis. International Ophthalmology. 2009 Feb 4;30(2):149–73. doi:10.1007/s10792-009-9301-3.