Retina Case #2
Authors: Paige Campbell (1), Dr. Alexander Kaplan (2)
Affiliations: (1) University of Alberta (2) University of Toronto
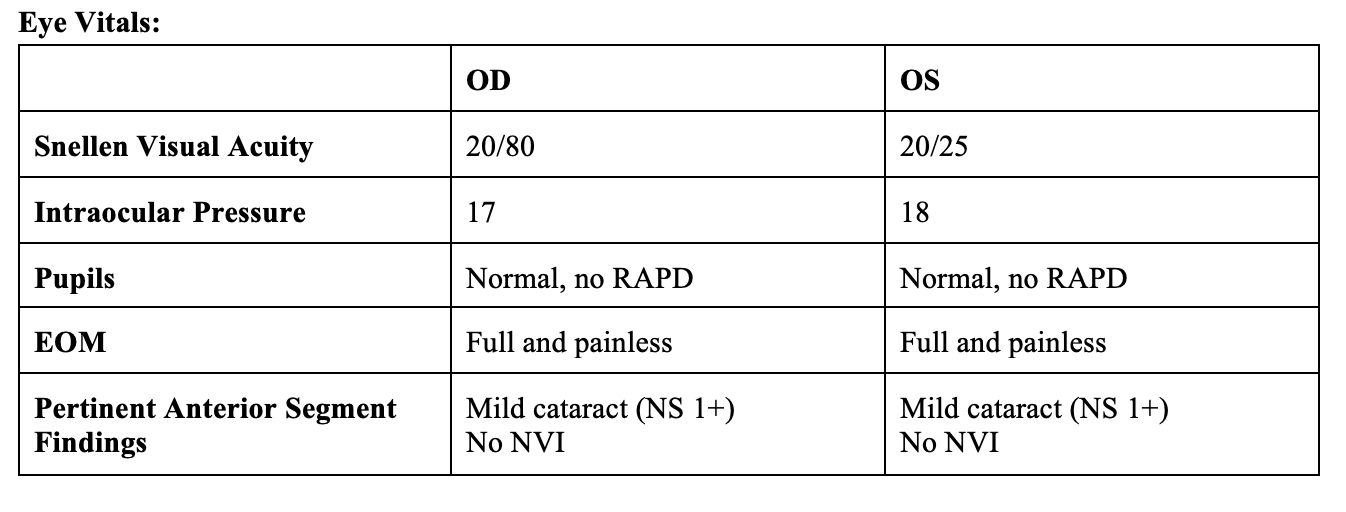
ID: 72F; referred for gradual onset of central vision distortion and blurring OD for 2 weeks
Past Ocular History: No significant myopia, no ocular trauma
Ocular gtts: None
Relevant Medical History: Hypertension (BP averages 140-150/90), and Hyperlipidemia
Medications: Amlodipine and Atorvastatin
-
IVFA OD at 8 seconds
Phase: Choroidal
Faint central hypofluorescence juxta-foveally (1), with subtle marginal hyperfluorescence (2).
-
IVFA OD at 20 seconds
Phase: Early ateriovenous
Defined juxta-foveal hyperfluorescence on the background of patchy choroidal hypofluorescence (3)
Borders sharply demarcated with evidence of early leakage (4)
-
IVFA at 35 seconds
Phase: Late arteriovenous
Increasing intensity and size of the central hyperfluorescence, with blurring of the margins secondary to leakage- classic “hot spot” appearance (3)
-
IVFA at 7 minutes
Phase: Late leakage
Intense hyperfluorescent macular-involving leakage (3)
Blurring and obscuration of lesion borders due to leakage (5)
Optic nerve: mild hyperfluorescence (6)
-
Diagnosis: Choroidal Neovascular Membrane (CNVM)
The findings are consistent with a classic choroidal neovascular membrane (CNVM). In the early phase, there was a well-defined hyperfluorescent membrane in the perifoveal region with sharp borders, characteristic of classic CNVM. During the mid-phase, the lesion showed progressive hyperfluorescence with mild leakage extending beyond its margins. By the late phase, there was intense leakage and pooling of dye, resulting in obscuration of the lesion borders.
-
The differential diagnosis for a classic (Type 2) CNVM includes:
Neovascular (wet) Age-Related Macular Degeneration (AMD) — most common cause in older adults
Myopic CNVM — associated with pathologic myopia
Angioid Streaks–related CNVM — in pseudoxanthoma elasticum, Ehlers-Danlos, Paget's
Inflammatory CNVM (Punctate Inner Choroidopathy, Multifocal Choroiditis) — usually younger patients with history of uveitis
Choroidal Rupture–associated CNVM — post-trauma
-
The patient present with intraretinal fluid, para-foveally on OCT without evidence of tractional changes (VMT, ERM) or obvious causes based on past medical history (no history of pseudophakia, no myopia, or diabetes). The IVFA becomes a tool to determine if there are sources and pattern of leakage in the parafoveal region.
Assess the location and extent of the neovascular membrane, especially if subfoveal involvement is suspected
Guide treatment planning (e.g., anti-VEGF therapy), ensuring appropriate targeting of active leakage
Rule out other mimickers such as central serous chorioretinopathy, retinal angiomatous proliferation, or polypoidal choroidal vasculopathy
-
Ruia S, Tripathy K. Fluorescein Angiography. [Updated 2023 Aug 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576378/
Mathis T, Holz FG, Sivaprasad S, Yoon YH, Eter N, Chen LJ, Koh A, Cunha de Souza E, Staurenghi G. Characterisation of macular neovascularisation subtypes in age-related macular degeneration to optimise treatment outcomes. Eye (Lond). 2023 Jun;37(9):1758-1765. doi: 10.1038/s41433-022-02231-y. Epub 2022 Sep 14. PMID: 36104522; PMCID: PMC10275926.