What Causes Hyperfluorescence?
Hyperfluorescence
-
Pre-injection fluorescence occurs when there is fluorescence in the images taken before the fluorescein dye is injected. The two primary causes of this are autofluorescence and pseudofluoresence.
-
Fluorescence that occurs prior to dye injection due to the presence of fluorophores such as lipofuscins or porphyrins.
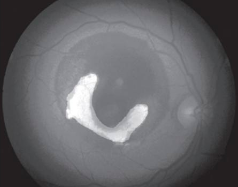
Optic disc drusen can have autofluorescence due to the presence of porphyrins in mitochondria and excessive mitochondria present in these drusen.
Retinal astrocytic hamartomas may also show autofluorescence.
-
Occurs due to the presence of old filters, allowing transmission of light outside of the specified blue and green wavelengths.
This can also be caused by dehemoglobinized blood which reflects blue light and will present as hyperfluorescence despite proper filters.
-
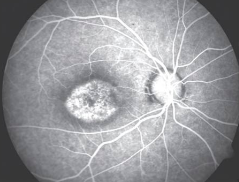
Transmitted fluorescence is also called a "window defect."
Healthy RPE usually block fluorescence from the choroidal vasculature, meaning RPE defects will result in choroidal hyperfluorescence. This may be caused by atrophy of the RPE layer or a congenital reduction in the pigment epithelium.
Hyperfluorescence occurs in the same shape as the RPE defect and does not increase in size or shape with time. This window defect fades as the dye washes out of choroidal circulation.
-
Usually this is caused by a pigment epithelial window defect.
Atrophy of pigment epithelium.
Congenital reduction in pigment epithelium.
-
A leak occurs when there is loss of fluorescein into the extracellular space. A full leak begins early in the scan and increases in size and intensity with time. Pooling and staining are types of leaks with defining characteristics explained below.
-
Defined as the accumulation of leaked fluorescein within a defined anatomical space. Once this defined space is filled, the margins in pooling remain constant and distinct throughout the study (unlike full leaking which continues to grow as the scan progresses).
-
Occurs in the recirculation phase, as fluorescein accumulates in collagen fibres. Structures that stain include the optic disc, Bruch's membrane, the sclera and large drusen. This is a physiologic cause of hyperfluorescence that is gradual and mild.
-
Neovascularization and fibrosis.
Intraocular inflammation.
Tumours of the disc, retina and choroid if the integrity of the retina has been interrupted.
-
There is usually leakage of the optic nerve head in healthy eyes because of the staining of the lamina cribrosa.
Increased hyperfluoresence of the disc can happen in papilledema, optic disc edema, optic nerve head drusen, tumours and vascular diseases related to the optic disc.
-
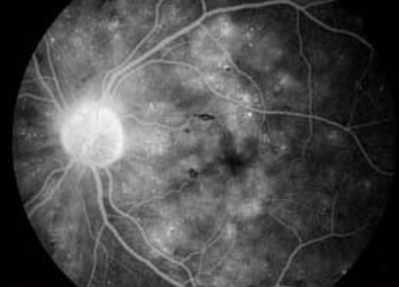
Cystoid appearance (inside the macula, aflower petal appearance because of the organization of the outer plexiform layer; outside of the macula, a honey- comb appearance): diabetic retinopathy, telangiectasis, choroidal or retinal inflammation, subretinal neovascularization, subretinal inflammation, choroidal tumours.
Non-cystoid pattern (usually due to small retinal vessel leakage): hypertension, diabetes, or vasculitis.
-
Given that the dye illuminates retinal vessels well, it is quite easy to determine the presence of abnormal retinal vasculature.
-
Tortuosity and dilation: Think diabetes or vascular occlusion.
Collaterals and Shunts: classify as arterial, arterio-venous or venous-venous.
Neovascularization: classify it as in the posterior pole or periphery. Think of diabetes, sickle cell disease, vascular occlusions, retinopathy of prematurity.
Aneurysms: microanuerysms from diabetes or vein occlusion or larger aneurysms like in tumours, Coat's, Leber's and macular telangiectasis.
-
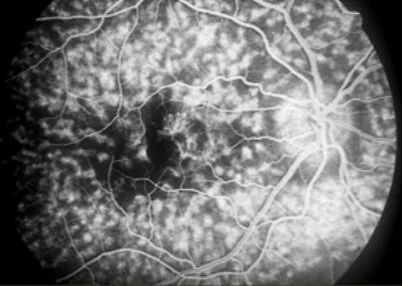
Although the choroid is better assessed using ICGA, early lacy hyperfluorescence may be seen on IVFA. It represents subretinal neovascularization.
The differential for subretinal neovascularization includes: retinochoroidal tumours, choroidal tumours, exudative macular degeneration, angioid streaks, histoplasmosis, myopia and choroidal rupture.
Figure informed by: Rabb MF, Burton TC, Schatz H, Yannuzzi LA. Fluorescein angiography of the fundus: a schematic approach to interpretation. Survey of ophthalmology. 1978 May 1;22(6):387-403.